Well, I've found the flaw in my training plan. My kids have swimming lessons on Friday afternoon. The younger three are together in a beginner class with 10 students and 1 teacher. It wasn't going to work, so I volunteered to assist. After 30 minutes, I'm exhausted. And of course, swimming is between my short-long run Friday mornings and my long-long run Saturday mornings. I was so tired this morning, I forgot to turn around and ended up doing an extra quarter mile! Oh, well, on race weekend when I *don't* have to swim between runs, I'll be that much more prepared, right?
Now for some good news: I haven't had any discomfort in my foot during my last three long runs! I think it's finally healed. Just in time, too, because I'm heading into high mileage. I did 7 miles yesterday and 14 today. Only 8 weeks until race day(s)! And now I think it's time for a nap.
Saturday, November 17, 2012
Saturday, October 27, 2012
Lighting a Candle
*Note: I intended to post this on October 15 for Pregnancy and Infant Loss Rememberance Day. Better late than never, right?
 Last night I heard a friend is pregnant. My first thought was to wish her a long and boring pregnancy, but I wasn't sure she'd get what I meant. Another friend is in her 41st week. She might consider my blessing more of a curse at this point. :) But anyone who has known the heartbreak of a non-boring pregnancy that ended too soon can relate. Being 41+3 weeks pregnant and miserable sounds pretty good to me!
Last night I heard a friend is pregnant. My first thought was to wish her a long and boring pregnancy, but I wasn't sure she'd get what I meant. Another friend is in her 41st week. She might consider my blessing more of a curse at this point. :) But anyone who has known the heartbreak of a non-boring pregnancy that ended too soon can relate. Being 41+3 weeks pregnant and miserable sounds pretty good to me!
As for losing a child before birth, well, for too long that just wasn't talked about. Things have started to change, but pregnancy loss is still taboo for a lot of people.
I want to tread carefully here. Some women (like me) choose to be very open about their pregnancy losses and grief. Others choose to grieve privately. Still others don't feel much grief at all, especially if the loss was very early. All of these responses are okay. There is no one right way to grieve, and I would never presume to tell a woman how to feel. I expect the same consideration. I fear there are many women who suffer in silence not because that's how they prefer to grieve but because it's what is expected of them.
On October 15, I lit two candles for my angels, Grace and Ian. I wish peace to all mothers (and fathers, too) who are missing babies.
 Last night I heard a friend is pregnant. My first thought was to wish her a long and boring pregnancy, but I wasn't sure she'd get what I meant. Another friend is in her 41st week. She might consider my blessing more of a curse at this point. :) But anyone who has known the heartbreak of a non-boring pregnancy that ended too soon can relate. Being 41+3 weeks pregnant and miserable sounds pretty good to me!
Last night I heard a friend is pregnant. My first thought was to wish her a long and boring pregnancy, but I wasn't sure she'd get what I meant. Another friend is in her 41st week. She might consider my blessing more of a curse at this point. :) But anyone who has known the heartbreak of a non-boring pregnancy that ended too soon can relate. Being 41+3 weeks pregnant and miserable sounds pretty good to me!
Speaking in general terms, it seems our society doesn't handle death very well. We expect the bereaved to keep a stiff upper lip, put on a brave face, and get on with their lives. We definitely don't want to be reminded of our own mortality or be made uncomfortable in any way. This is bad enough when someone has lost an adult friend or family member, but it's even worse when a child dies. Children aren't supposed to die.
As for losing a child before birth, well, for too long that just wasn't talked about. Things have started to change, but pregnancy loss is still taboo for a lot of people.
I want to tread carefully here. Some women (like me) choose to be very open about their pregnancy losses and grief. Others choose to grieve privately. Still others don't feel much grief at all, especially if the loss was very early. All of these responses are okay. There is no one right way to grieve, and I would never presume to tell a woman how to feel. I expect the same consideration. I fear there are many women who suffer in silence not because that's how they prefer to grieve but because it's what is expected of them.
On October 15, I lit two candles for my angels, Grace and Ian. I wish peace to all mothers (and fathers, too) who are missing babies.
Saturday, October 13, 2012
Running in the Rain
Today was a perfect running day. All of my best runs, training or race day, have come in rainy weather with just a bit of wind and temperatures in the 40s and 50s. As I headed out this morning, it had been sprinkling off an on. It started raining around mile 2 and kept getting heavier and heavier until around mile 6 it was a torrential downpour! I loved it, couldn't stop smiling and laughing. Yeah, I know I'm goofy. I have to be, right, to be training for the Goofy Challenge?
This weekend was my second of back to back long runs. Last week, I did 3 miles on Friday and 6 on Saturday. Yesterday I did 4 with another 8 today. Next week I plan to do 5 on Friday and 10 on Saturday, followed by a "cut back" rest week.
This weekend was my second of back to back long runs. Last week, I did 3 miles on Friday and 6 on Saturday. Yesterday I did 4 with another 8 today. Next week I plan to do 5 on Friday and 10 on Saturday, followed by a "cut back" rest week.
Wednesday, October 10, 2012
Nine Years
Nine years ago today, the course of my life changed forever. I went to the OB's office that afternoon to follow up on what we thought was an allergy attack. Instead I was diagnosed with preeclampsia. He wouldn't even let me drive myself to the hospital, asking a nurse to take me instead. Once there, we found I had cerebral edema (brain swelling) and was at very high risk for seizure or stroke. I was also in heart failure and struggling to get oxygen even with a mask on. My liver was heading toward failure, my kidneys were struggling, and my blood cell counts were dropping quickly. Long story short, I would die unless my baby was born in the next 48 hours.
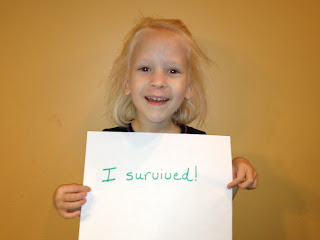
My baby and I both survived, for which I praise God. She will be nine on Friday, and has grown into such a lovely young lady. As for me, I have become active with the Preeclampsia Foundation, raising awareness so others can get the care they need and raising money for research into better detection, treatment, and maybe even prevention/cure. If you had told me 10 years ago that pregnancy, birth, and breastfeeding would be my passion I'd have thought you were crazy. But here I am, all thanks to that moment nine years ago.
Thursday, October 4, 2012
It's Been a While
A lot has happened in the 7 weeks since my marathon, and blogging has temporarily fallen by the wayside. The biggest thing is that I had surgery 2 weeks ago. This happened rather suddenly (went from no symptoms to debilitating pain in 5 weeks) and has set me back in a lot of ways, but I'm heading in the right direction again. The surgery was unrelated to my foot injury, by the way, but a silver lining is that I've been mostly off my foot for a while and has improved a lot. I still get a twinge or two when I run, but no outright pain.
I started back with light training this week, walking 2 miles on Saturday, Monday, and Wednesday. I'm planning another 3 tomorrow and, if all goes well, 5 or 6 Saturday. I think I can keep ahead of the Disney Goofy cutoff time (16min/mile pace) even if I just walk, or with just a little running built in. I've already paid the money, so I'll do whatever I need to do to get those medals!
I hope to be more active again on the ol' blog. I've got a couple posts mostly written, just need to touch them up a bit. To look for this month: another bra review, thoughts on Pregnancy and Infant Loss Rememberance Month, and issues of informed consent.
I started back with light training this week, walking 2 miles on Saturday, Monday, and Wednesday. I'm planning another 3 tomorrow and, if all goes well, 5 or 6 Saturday. I think I can keep ahead of the Disney Goofy cutoff time (16min/mile pace) even if I just walk, or with just a little running built in. I've already paid the money, so I'll do whatever I need to do to get those medals!
I hope to be more active again on the ol' blog. I've got a couple posts mostly written, just need to touch them up a bit. To look for this month: another bra review, thoughts on Pregnancy and Infant Loss Rememberance Month, and issues of informed consent.
Wednesday, September 5, 2012
Volunteer Profile: Marathon Runner
Volunteer Profile: Marathon Runner
How cool is this? I'm the featured volunteer in the September newsletter for the Preeclampsia Foundation!
How cool is this? I'm the featured volunteer in the September newsletter for the Preeclampsia Foundation!
Wednesday, August 22, 2012
Leading Ladies Race Report
So this is a rather sad race report because it ends with a DNF (did not finish). As you know, I injured my foot a few weeks before race day. My doctor had cleared me to run, and I spent a frantic few days trying to get my leg loosened up after 11 days on crutches.
My mom and I left early Friday morning for the 15 hour drive to Spearfish, SD. We spent Saturday walking around Mt Rushmore and picking up my packet at the Expo. I got a $500 gift card in my goody bag! I must have gotten the lucky bag, because that's a lot of money to give 700 participants. I also got to meet Yolanda Holder, who has the Guiness World Record for most marathons run by a woman in one calendar year (106). She's in the process of breaking her own record, and Leading Ladies was number 67 for the year. I got an autographed copy of her book. Really cool!
I got up around 3:30 Sunday morning and headed to the bus that would take me to the start line. It was about 55 degrees outside, not bad running weather. And then we drove 3000 feet up the mountain, where it was 42. Brr! I like running in the cold, but as the sun came up the temperature in the canyon quickly warmed up to almost 80. The wide range of temperatures was pretty difficult on top of everything else.
I started off slow but picked up the pace as my muscles loosened up. Things seemed to be going well, except for one problem. I had pain with every. single. step. It wasn't what I would call a "damage" pain, but it was uncomfortable. Despite that, I was still doing really well, finishing the first half in an even 3 hours.
I really enjoyed the beautiful course. There was a mountain stream next to the road for the first half, and you could hear it bubbling. There was a fresh pine scent in the air, and you could see the sunshine move its way down to the bottom of the canyon. This song kept running through my head as I ran.
It was so disappointing not to finish. However, 23 miles in 5:30ish on a bad foot is pretty awesome! As they say in Boston, I am wicked hard core. Thinking of my PE Sisters really helped me push through as far as I did. The race director still made sure I got a medal and a rose.
Mom and I headed back to the hotel for a quick shower, then had a 15 hour drive home so Mom could get to work Monday. I'm mostly recovered. My foot still aches, but hopefully is heading in the right direction. I'm taking a few weeks off before I start training for my next race, and I'll do that very carefully.
The most important thing is that I raised $4000 for the Preeclampsia Foundation. Thanks to all who donated and who prayed for and encouraged me during my training.
One more item of business. Since I did not have a finish time, I put the names of everyone who had submitted a guess into a hat, and Smartie pulled out Melodee! Mel, I'll make sure to give you your gift card on Friday when I see you.
My mom and I left early Friday morning for the 15 hour drive to Spearfish, SD. We spent Saturday walking around Mt Rushmore and picking up my packet at the Expo. I got a $500 gift card in my goody bag! I must have gotten the lucky bag, because that's a lot of money to give 700 participants. I also got to meet Yolanda Holder, who has the Guiness World Record for most marathons run by a woman in one calendar year (106). She's in the process of breaking her own record, and Leading Ladies was number 67 for the year. I got an autographed copy of her book. Really cool!
I got up around 3:30 Sunday morning and headed to the bus that would take me to the start line. It was about 55 degrees outside, not bad running weather. And then we drove 3000 feet up the mountain, where it was 42. Brr! I like running in the cold, but as the sun came up the temperature in the canyon quickly warmed up to almost 80. The wide range of temperatures was pretty difficult on top of everything else.
I started off slow but picked up the pace as my muscles loosened up. Things seemed to be going well, except for one problem. I had pain with every. single. step. It wasn't what I would call a "damage" pain, but it was uncomfortable. Despite that, I was still doing really well, finishing the first half in an even 3 hours.
I really enjoyed the beautiful course. There was a mountain stream next to the road for the first half, and you could hear it bubbling. There was a fresh pine scent in the air, and you could see the sunshine move its way down to the bottom of the canyon. This song kept running through my head as I ran.
 |
| Horrible pic, I was crying |
While very beautiful, the course was absolutely brutal for someone with an injured foot. Because it's so small, and because it's run on a scenic tourist drive, they did not close down the road for this race. We had to run on the far left side of the road. If you've ever run on a highway, especially on a banked curve, you know it angles down at the sides. My bad foot was turned at an angle the whole way, putting the most pressure on the worst possible spot. I tried to move toward the center of the road where it's flatter when I could, but a car would always come along right as I got into a rhythm. I also tried running in the grass next to the road, and that was my undoing. Just after the 21 mile marker, I stepped on a clod of dirt directly under the spot where it hurts. I had immediate sharp pain that continued for the rest of the race. I had to walk another two miles to get to the next aid station, where I asked the ambulance for a ride to the finish.
It was so disappointing not to finish. However, 23 miles in 5:30ish on a bad foot is pretty awesome! As they say in Boston, I am wicked hard core. Thinking of my PE Sisters really helped me push through as far as I did. The race director still made sure I got a medal and a rose.
Mom and I headed back to the hotel for a quick shower, then had a 15 hour drive home so Mom could get to work Monday. I'm mostly recovered. My foot still aches, but hopefully is heading in the right direction. I'm taking a few weeks off before I start training for my next race, and I'll do that very carefully.
The most important thing is that I raised $4000 for the Preeclampsia Foundation. Thanks to all who donated and who prayed for and encouraged me during my training.
One more item of business. Since I did not have a finish time, I put the names of everyone who had submitted a guess into a hat, and Smartie pulled out Melodee! Mel, I'll make sure to give you your gift card on Friday when I see you.
Thursday, August 16, 2012
Guess My Finish Time
It's time for another game of Guess My Finish Time. All you have to do is leave a comment under this post by 6:00am CST Sunday (the start of the race) with your guess in hours:minutes (and I guess seconds if you want to be that specific). Price is Right rules are in effect--closest without going over. Winner gets a $10 gift card to Starbucks. Encouragement is appreciated.
I got four miles in tonight, and it went much better than yesterday. Still not great, but I'm not *quite* as terrified of the bus of shame. If I were healthy, I'd be shooting for a finish time of 5:50. Running wounded, I think anything under 6:30 would be pretty darn good, and as long as I'm under the 7:00 cut off, I'll be happy.
It looks like I'll only have roaming service for my phone, so I probably won't update until I get home Monday. Can't wait to post my successful race report!
I got four miles in tonight, and it went much better than yesterday. Still not great, but I'm not *quite* as terrified of the bus of shame. If I were healthy, I'd be shooting for a finish time of 5:50. Running wounded, I think anything under 6:30 would be pretty darn good, and as long as I'm under the 7:00 cut off, I'll be happy.
It looks like I'll only have roaming service for my phone, so I probably won't update until I get home Monday. Can't wait to post my successful race report!
Wednesday, August 15, 2012
It's Not Broken!
 Yep, we're dancing here! I spent 11 days on crutches thinking it was likely my foot was broken, but praying desperately it wasn't. I figured if it was broken, I'd be ahead of the game on healing, and if it wasn't, I was only inconveniencing myself.
Yep, we're dancing here! I spent 11 days on crutches thinking it was likely my foot was broken, but praying desperately it wasn't. I figured if it was broken, I'd be ahead of the game on healing, and if it wasn't, I was only inconveniencing myself.
I had an MRI yesterday, and the tech (with a lot of disclaimers) said she couldn't see a break. I tentatively started walking on my foot last night. Wow. My ankle feels weak and my whole leg is stiff.
I got the official call this morning. Doctor says it's not broken and to go ahead and enjoy my race! After screaming, texting my family, and posting on Facebook, I got right on the treadmill for an easy mile. I did another mile this afternoon, then met up with my team and coaches this evening. We worked out a plan for the next few days, and I did another two miles with them.
Now my right leg from toe to lower back is so stiff and tight it feels like I've already run the marathon, while my left side could easily go another ten miles. This is not going to be a pretty race, but that's okay. A finish is a win. As long as I can get across the finish line within the 7 hour time limit, I'll sing all the way home.
Thanks to everyone who prayed over the last two weeks, and if you feel so moved, I'd appreciate more prayers over the next few days as I rehab and then run.
Friday, August 3, 2012
This is a Nightmare
After a really awesome 20 mile run on Saturday with minimal discomfort, my foot started hurting Monday. Like, really bad and getting worse. So I went to the doctor today, and he said if it were up to him, he'd assume it's a stress fracture and boot me for six weeks. But since I REALLY, REALLY want to run my race in two weeks, he ordered an x-ray and MRI. The x-ray had no obvious fracture. The MRI is scheduled for the 13th, and in the mean time I'm staying off my feet as much as possible (says the mom of four active children!) I'm holding out hope that I can still run, or at least walk at least the Half. This is just terrible timing.
Saturday, July 28, 2012
Twenty Miles DONE!
I'm three weeks out from race day, and today was my longest training run. I did 20 miles and a bit in 4:37:50, which was ahead of my goal of 4:40. Plus I had negative splits, which means I was faster as I went on! My first 5 mile leg was 1:10, second and third also 1:10 but both included bathroom breaks, and last leg in 1:08. I feel good, no pain, still smiling at the end. I'm ready!
I've raised $3600 for the Preeclampsia Foundation. A few people have mentioned still wanting to donate, but I don't think I'll reach my $5000 goal. That's okay, $3600 is still a good amount. If anyone still wishes to donate, click on the What AM I Running For tab at the top of the page for instructions.
I've raised $3600 for the Preeclampsia Foundation. A few people have mentioned still wanting to donate, but I don't think I'll reach my $5000 goal. That's okay, $3600 is still a good amount. If anyone still wishes to donate, click on the What AM I Running For tab at the top of the page for instructions.
Friday, July 27, 2012
Happy Birthday, Ian
Yesterday started with a poor night's sleep: three nightmares. We kept busy with lots of activities, but the busyness couldn't drown out the memories. Last night, as I held the boy who Is snuggled in my arms, I thought of the boy who Was, who I held in the palm of my hand four years ago.
He was meant to be, but not meant to stay. His short time on Earth left a deep scar on my heart.
He'd probably have blond hair and blue eyes like his sisters and brother. I wonder if he'd be a daredevil like his brother, running at 10 months, jumping off the piano at 12 months, making it all the way across the monkey bars at 18 months. Or would he be more studious, a builder, a thinker? Would he run the track with his daddy? Would he read books with me? Would he dress up and paint his nails with his sisters, then turn around and climb a tree?
Most of all, I wonder if he knows how much I love him, how much I wanted him, and how much I still grieve for him. Can he see me from Heaven? Is he with his sister, my other lost angel?
Ian (and Grace), Mama loves you so much. I long for the day I can finally hold you again.
I finally fell asleep, only to have more nightmares. I couldn't work up the energy to run yesterday, and I'll need to rest today to prepare for my 20 mile training tomorrow. I'll be carrying my angels in my heart to get me through.
Tuesday, July 17, 2012
And I would walk 500 miles...
This song has been stuck in my head this week, for a very good reason! I've officially reached the halfway mark on my goal for the year: 508 miles done, 492 (or more) to go!
Wednesday, July 11, 2012
A Hard Day
The month of July starts off so well: our wedding anniversary is June 30th, and then the twins' birthday is July 7th. And then the 11th comes around. This was the estimated due date of my second child, who died in the first trimester. We named "her" Grace. She would have turned six this year.
As hard as this day is, I know the 26th will be harder. That's the day I lost my fourth child, Ian. I still can't bring myself to talk about much of the details of that day. I'm dreading the next two weeks. And that's all I have to say about that.
As hard as this day is, I know the 26th will be harder. That's the day I lost my fourth child, Ian. I still can't bring myself to talk about much of the details of that day. I'm dreading the next two weeks. And that's all I have to say about that.
Saturday, June 30, 2012
Survivor Saturday: Meghan's Story
I'm sitting here with my foot in a bucket of ice water, having just completed 10 miles in honor of Meghan and her baby. I've had to switch to a less agressive training schedule after re-injuring my ankle. I'm confident I will finish Leading Ladies, but I may be a bit slower than I'd hoped. The ankle is improving, and I was able to do all of my run intervals today, which is a huge improvement over last week where I walked four of six miles.
If you are a survivor of Preeclampsia or a related condition, I would love to share your story and to run in your honor. Stories can be submitted to whatyourunningfor@gmail.com . The more women know about PE, the better they can advocate for themselves and their children.
Meghan shared her story with me this week. She is a fellow runner who had preeclampsia. She includes some great tips for pregnant women and PE survivors.
I am a runner. I have run one marathon and about a half dozen half marathons since I began running for the sake of running in 2004, right before my 30th birthday. I have run 80 miles a week before (plus road
biking and distance swimming), and when I became pregnant with my daughter, I was running about 40 miles a week, while also swimming 1-2 miles at a time and road biking. I was fit, but in a healthy way -
something that had not always been the case. I always felt it was not worth going for a run for less than 6-7 miles - until I was pregnant. Those 3-6 mile runs were exhausting but exhilarating at the same time
- I had never worked so hard to put one foot in front of the other, yet be going so slowly. The fact that my legs were carrying my daughter and me over those miles, with my belly growing, was beautiful to me - and probably a little concerning for the random person who drove by.
I started wearing maternity clothes just before 7 weeks gestation. I literally gained a pound a week from moment one. You could tell how many weeks gestation I was not by my uterine height, but by how many
pounds I had gained. At 18 weeks gestation, while climbing a flight of stairs at work, I started to have contractions - and not just Braxton Hicks contractions. My headache from first trimester also returned
(gosh, it must just be that hormone headache I thought), and as the weeks went on, I was gaining 4 or more pounds a day at work, and then I would lose it the next 3-4 days while at home, laying down. I had squigglies at the top of my vision while I was out running and sometimes while laying down, and my contractions were continuing and getting more constant. At 26 weeks gestation, while at work as a
Pediatric Nurse Practitioner in a Family Birthing Center, my contractions started to wrap around my body and lasted for 45 seconds every 2-3 minutes, so I called the OB on call. Instead of staying at
my hospital, I traveled to the hospital that I was going to deliver at, which in the end, was a mistake. My blood pressure there was 150s-160s/90s-100s after I had always been 90s/50s, and the
contractions showed up nicely on the monitor. After a few doses of tocolytics and me laying on my left side, the contractions slowed and my blood pressure came down (of course), so they sent me home to do a 24 hour urine. I dropped it off about 30 hours later after fighting with the lab to accept it because my providers had not given me an outpatient lab slip. Little did I know that this was going to be the
first of many mistakes.
Speed ahead 9 weeks: after 9 weeks of continual contracting and hypertension and headaches and visual disturbances and not getting anywhere with my complaints, I am seen by the Nurse Practitioner on an urgent visit for my visual changes getting worse. I have spent these last 9 weeks on self-imposed bedrest when I was not working my 24 hour shifts, because my contractions are unstoppable, I have dilated some, but no one will officially put me on bed rest. I am admitted to the hospital with pre-eclampsia. Turns out my 24 hour urine 9 weeks earlier, along with my hypertension and symptomology, have diagnosed me - and no one acted on any of this. I repeat a 24 hour urine and it is higher this time. I am finally officially placed on bed rest, but sent home. At this point, I am supposed to return if I feel sicker. Honestly, I think I felt sicker, but you are already so sick that your brain is not working (beyond the normal pregnancy brain issues). I am seen at my regular OB appointment 5 days later and am sent immediately to the hospital for induction for severe preeclampsia. The first induction fails, probably secondary to inaccurate Cervidil placement, and I am re-induced. My daughter is born on my 35th birthday after 51 hours of induction and eventual cesarean section secondary to cephalopelvic disproportion after two failed vacuum attempts. She had crowned at 1.5 hours of me pushing, but 3.5 hours after that, she was still only crowned and stuck on my coccyx. The OBs (there were three of them at this point, plus two residents) pushed her back up into my uterus in the surgical suite, thereby completely lacerating/rupturing my cervix and part of my lower uterine segment. She was born healthy despite two severe episodes of bradycardia during my epidural administration and reinforcement, which was the result of my hypotension and loss of consciousness.
She is now two years old, and has a gross motor delay and an expressive language delay, and is seen by Birth to 3, our early intervention program. She is smart and lively - with fine motor skills and receptive language skills being at or above average. Her speech is improving every day, but I waited until the month before her second birthday to hear the sweetest words - "mama." Her gross motor deficits are probably the result of low core tone, and we are also working to improve that.
I had postpartum preeclampsia, along with a host of other issues. I was on blood pressure medications for the year after delivery. I have labile blood pressures now, but am not on any medications. I began running again about 9 weeks after delivery - my first run was 2 miles and it felt great to be pushing that jogger. I was up to 7.5 miles at 7 months postpartum, but we had a horrible winter that I could not take the jogger out onto the road, and I did not make it to the gym, so I lost that fitness over the winter. That next spring I was up to 5.5 miles within a month of running again, and then had a subchondral fracture of my ankle, so I had to take 6 months off running and walking and could not get out with a bike due to my husband's schedule. In more fits and starts, vaccine-not-covered influenza took its toll on me this winter when we finally got a treadmill, but I am now back at it with renewed committment. I am still a runner, even if I am barely getting in three miles a run a couple of times a week. Now, more than ever, any amount of running is worth it.
Pieces of advice for all pregnant women:
1) your spot-check urine does not have to have any protein on it for you to be preeclamptic - I was always negative because I hydrated myself so well and my kidneys just put all that back out there - the 24 hour urine is usually the gold standard, although some studies show a creatinine clearance ratio can be accurate.
2) your blood pressure is not accurate laying on your left side, with a cuff too big for you, with a person not carefully taking it - I never had hypertension in my OBs office unless the Nurse Practitioner or MD took it, but always had it at the hospital when I arrived for my contractions becoming intolerable (and my fetal fibronectin expiring) and I always had it at home.
3) don't be afraid to fire your OB - I wish I had when I miscarried prior to the preeclamptic pregnancy, and had a tech come in and ask when my last period was, what I was using for birth control etc, when I was there as a post-miscarriage appointment. After my delivery, and finding out when I requested my records about all the mistakes made, I did fire my OB.
4) don't be afraid to demand a second opinion with a Maternal Fetal Medicine specialist/Perinatologist - I wish I had, but I listened to the reassurance provided by my providers and did not go with my gut
feeling.
5) don't take any lip from the L&D nurses - I would rather be a "frequent flyer" than die or have my baby die.
6) educate yourself.
Pieces of advice for preeclampsia survivors:
1) see a MFM/Perinatologist after your pregnancy and before another pregnancy - make sure you have a plan of care for the subsequent pregnancy
2) know your risk factors for future health issues and modify as many of them as you can
3) grieve what you have lost
4) look to the future
5) educate your son and daughter for their futures
6) talk about this so more women are aware
If I had a chance to do it all over again, I would be much more pushy to my providers, and I would tell my husband to do the same. I knew what preeclampsia was. I knew I had it. I expressed this to my
providers, but I was not able to be a great advocate for myself because I was already too sick and figured my providers knew better than I did. As a result of my early preeclampsia, my husband and I
were very fearful of having another pregnancy, but were going to go ahead and have another with some very close medical care. As a result of my cervical injury and my investigation into my now incompetent cervix, I found AbbyLoopers and its experts on transabdominal cervical cerclage. Although it is an option for me, combined with another type of cerclage during pregnancy, my husband and I feel that, combined with the early preeclampsia, my cervical injury and the plan for a subsequent pregnancy, it is too risky for us, so we have decided to not have another child. Today, 26 months after the birth of my daughter, I still cry about this. I do cherish what I have with her and try not to let worry and fear and anger overcome all that I have.
If you are a survivor of Preeclampsia or a related condition, I would love to share your story and to run in your honor. Stories can be submitted to whatyourunningfor@gmail.com . The more women know about PE, the better they can advocate for themselves and their children.
Meghan shared her story with me this week. She is a fellow runner who had preeclampsia. She includes some great tips for pregnant women and PE survivors.
Meghan's Story
I am a runner. I have run one marathon and about a half dozen half marathons since I began running for the sake of running in 2004, right before my 30th birthday. I have run 80 miles a week before (plus road
biking and distance swimming), and when I became pregnant with my daughter, I was running about 40 miles a week, while also swimming 1-2 miles at a time and road biking. I was fit, but in a healthy way -
something that had not always been the case. I always felt it was not worth going for a run for less than 6-7 miles - until I was pregnant. Those 3-6 mile runs were exhausting but exhilarating at the same time
- I had never worked so hard to put one foot in front of the other, yet be going so slowly. The fact that my legs were carrying my daughter and me over those miles, with my belly growing, was beautiful to me - and probably a little concerning for the random person who drove by.
I started wearing maternity clothes just before 7 weeks gestation. I literally gained a pound a week from moment one. You could tell how many weeks gestation I was not by my uterine height, but by how many
pounds I had gained. At 18 weeks gestation, while climbing a flight of stairs at work, I started to have contractions - and not just Braxton Hicks contractions. My headache from first trimester also returned
(gosh, it must just be that hormone headache I thought), and as the weeks went on, I was gaining 4 or more pounds a day at work, and then I would lose it the next 3-4 days while at home, laying down. I had squigglies at the top of my vision while I was out running and sometimes while laying down, and my contractions were continuing and getting more constant. At 26 weeks gestation, while at work as a
Pediatric Nurse Practitioner in a Family Birthing Center, my contractions started to wrap around my body and lasted for 45 seconds every 2-3 minutes, so I called the OB on call. Instead of staying at
my hospital, I traveled to the hospital that I was going to deliver at, which in the end, was a mistake. My blood pressure there was 150s-160s/90s-100s after I had always been 90s/50s, and the
contractions showed up nicely on the monitor. After a few doses of tocolytics and me laying on my left side, the contractions slowed and my blood pressure came down (of course), so they sent me home to do a 24 hour urine. I dropped it off about 30 hours later after fighting with the lab to accept it because my providers had not given me an outpatient lab slip. Little did I know that this was going to be the
first of many mistakes.
Speed ahead 9 weeks: after 9 weeks of continual contracting and hypertension and headaches and visual disturbances and not getting anywhere with my complaints, I am seen by the Nurse Practitioner on an urgent visit for my visual changes getting worse. I have spent these last 9 weeks on self-imposed bedrest when I was not working my 24 hour shifts, because my contractions are unstoppable, I have dilated some, but no one will officially put me on bed rest. I am admitted to the hospital with pre-eclampsia. Turns out my 24 hour urine 9 weeks earlier, along with my hypertension and symptomology, have diagnosed me - and no one acted on any of this. I repeat a 24 hour urine and it is higher this time. I am finally officially placed on bed rest, but sent home. At this point, I am supposed to return if I feel sicker. Honestly, I think I felt sicker, but you are already so sick that your brain is not working (beyond the normal pregnancy brain issues). I am seen at my regular OB appointment 5 days later and am sent immediately to the hospital for induction for severe preeclampsia. The first induction fails, probably secondary to inaccurate Cervidil placement, and I am re-induced. My daughter is born on my 35th birthday after 51 hours of induction and eventual cesarean section secondary to cephalopelvic disproportion after two failed vacuum attempts. She had crowned at 1.5 hours of me pushing, but 3.5 hours after that, she was still only crowned and stuck on my coccyx. The OBs (there were three of them at this point, plus two residents) pushed her back up into my uterus in the surgical suite, thereby completely lacerating/rupturing my cervix and part of my lower uterine segment. She was born healthy despite two severe episodes of bradycardia during my epidural administration and reinforcement, which was the result of my hypotension and loss of consciousness.
She is now two years old, and has a gross motor delay and an expressive language delay, and is seen by Birth to 3, our early intervention program. She is smart and lively - with fine motor skills and receptive language skills being at or above average. Her speech is improving every day, but I waited until the month before her second birthday to hear the sweetest words - "mama." Her gross motor deficits are probably the result of low core tone, and we are also working to improve that.
I had postpartum preeclampsia, along with a host of other issues. I was on blood pressure medications for the year after delivery. I have labile blood pressures now, but am not on any medications. I began running again about 9 weeks after delivery - my first run was 2 miles and it felt great to be pushing that jogger. I was up to 7.5 miles at 7 months postpartum, but we had a horrible winter that I could not take the jogger out onto the road, and I did not make it to the gym, so I lost that fitness over the winter. That next spring I was up to 5.5 miles within a month of running again, and then had a subchondral fracture of my ankle, so I had to take 6 months off running and walking and could not get out with a bike due to my husband's schedule. In more fits and starts, vaccine-not-covered influenza took its toll on me this winter when we finally got a treadmill, but I am now back at it with renewed committment. I am still a runner, even if I am barely getting in three miles a run a couple of times a week. Now, more than ever, any amount of running is worth it.
Pieces of advice for all pregnant women:
1) your spot-check urine does not have to have any protein on it for you to be preeclamptic - I was always negative because I hydrated myself so well and my kidneys just put all that back out there - the 24 hour urine is usually the gold standard, although some studies show a creatinine clearance ratio can be accurate.
2) your blood pressure is not accurate laying on your left side, with a cuff too big for you, with a person not carefully taking it - I never had hypertension in my OBs office unless the Nurse Practitioner or MD took it, but always had it at the hospital when I arrived for my contractions becoming intolerable (and my fetal fibronectin expiring) and I always had it at home.
3) don't be afraid to fire your OB - I wish I had when I miscarried prior to the preeclamptic pregnancy, and had a tech come in and ask when my last period was, what I was using for birth control etc, when I was there as a post-miscarriage appointment. After my delivery, and finding out when I requested my records about all the mistakes made, I did fire my OB.
4) don't be afraid to demand a second opinion with a Maternal Fetal Medicine specialist/Perinatologist - I wish I had, but I listened to the reassurance provided by my providers and did not go with my gut
feeling.
5) don't take any lip from the L&D nurses - I would rather be a "frequent flyer" than die or have my baby die.
6) educate yourself.
Pieces of advice for preeclampsia survivors:
1) see a MFM/Perinatologist after your pregnancy and before another pregnancy - make sure you have a plan of care for the subsequent pregnancy
2) know your risk factors for future health issues and modify as many of them as you can
3) grieve what you have lost
4) look to the future
5) educate your son and daughter for their futures
6) talk about this so more women are aware
If I had a chance to do it all over again, I would be much more pushy to my providers, and I would tell my husband to do the same. I knew what preeclampsia was. I knew I had it. I expressed this to my
providers, but I was not able to be a great advocate for myself because I was already too sick and figured my providers knew better than I did. As a result of my early preeclampsia, my husband and I
were very fearful of having another pregnancy, but were going to go ahead and have another with some very close medical care. As a result of my cervical injury and my investigation into my now incompetent cervix, I found AbbyLoopers and its experts on transabdominal cervical cerclage. Although it is an option for me, combined with another type of cerclage during pregnancy, my husband and I feel that, combined with the early preeclampsia, my cervical injury and the plan for a subsequent pregnancy, it is too risky for us, so we have decided to not have another child. Today, 26 months after the birth of my daughter, I still cry about this. I do cherish what I have with her and try not to let worry and fear and anger overcome all that I have.
Saturday, June 16, 2012
Nine Weeks to Race Day
I finished a brutal 16 miles this morning. I was a lot slower than usual, and my muscles were threatening major cramps toward the end, but I finished without skipping a run interval. I did not receive a submission for today's Survivor Saturday. I still had a mother and children in mind, but I hesitate to share too many details without her permission. (We are no longer in touch.)
J lost her first son to PE at 22 weeks around the same time I was diagnosed with my twins, also at 22 weeks. We both found the amazing forums at the Preeclampsia Foundation. A few months later, she was pregnant with her second. We encouraged, supported, and prayed for each other through those long, stressful months. J had a beautiful, living son at 36 weeks with only mild PE. I cried when I read her birth announcement. A new pregnancy after previous complications and especially after a loss can be so stressful. Sharing it with women who understand helps a lot.
J lost her first son to PE at 22 weeks around the same time I was diagnosed with my twins, also at 22 weeks. We both found the amazing forums at the Preeclampsia Foundation. A few months later, she was pregnant with her second. We encouraged, supported, and prayed for each other through those long, stressful months. J had a beautiful, living son at 36 weeks with only mild PE. I cried when I read her birth announcement. A new pregnancy after previous complications and especially after a loss can be so stressful. Sharing it with women who understand helps a lot.
Tuesday, June 12, 2012
Still Looking for Survivor Stories
I've used all the stories submitted to me so far. I've had three people mention they had stories for me but haven't gotten around to writing them yet. I'd like to get enough to have one each Saturday until race day, so that's nine more. I dedicate my long run in honor of the featured mother and baby(ies) each week.
If your life has been affected by preeclampsia or related conditions, I would like to share your story. It's so important for pregnant women to know about the risks, the signs and symptoms, and what to expect. Stories can be submitted to whatyourunningfor@gmail.com. You can find other Survivor Stories here.
If your life has been affected by preeclampsia or related conditions, I would like to share your story. It's so important for pregnant women to know about the risks, the signs and symptoms, and what to expect. Stories can be submitted to whatyourunningfor@gmail.com. You can find other Survivor Stories here.
Monday, June 11, 2012
Sunday, June 10, 2012
Survivor Saturday: Jamie's Story
I'm a day late posting this, but I did run 8 miles in honor of Jamie and her children yesterday. Jamie's story shows how important it is to trust our instincts, and that high risk pregnancies should be handled by specialists. (I have a post planned for this week exploring that issue further.)
After about 1 ½ years of marriage my husband and I decided we were ready to have a baby. We were pregnant in no time and aside from the nausea and constant vomiting, I had a perfectly normal pregnancy until about 37 weeks. I thought I was going into labor and so I headed to labor and delivery to be checked out. I was not in labor, but my blood pressure was so high so I was kept overnight. I was sent home the next day on bedrest but went into labor that night and delivered a healthy 6 lb, 9 oz baby girl. We named her Carly. I was on the dreaded magnesium drip for 12 hours and then they turned it off. I was sent home without any instructions regarding what could happen after delivery... or that this same scenario could repeat itself in my next pregnancy.
Fast forward about 2 ½ years and we decided we were ready to give Carly a sibling. After a year of trying we were finally pregnant again. We live in a very small town and it is common here for people to use their family practice doctor as their OB. Since things had gone ok the first time I had no reason to believe things wouldn’t go the same way the second time. So off I went, back to my family practice doctor. Things were fairly routine again up until about 23 weeks. I was at work and started having contractions. I was very unconcerned at first and decided I just needed to drink some water and rest. I did but the contractions did not stop. I am an RN and worked at a hospital in a larger town about an hour away. It is important that I am a nurse because even with that education and experience I had no idea what could happen. I think we spent less than 30 minutes covering PE in nursing school and I worked in adult ICU and so we never deal with the women’s health side. In hindsight, I so wish I would have gone to labor and delivery where I worked instead of driving the hour home to go to the smaller hospital.
Oh hindsight is so very 20/20. Anyway, I drove home and went to L&D. At that time they did a fetal fibronectin test and noticed my pressures were a bit elevated. I was not seen by my doctor that day because he was not on call. The on call told me to go home on bedrest until the following Monday and then to follow up with my doctor for the test results. I did just as I was told. When I got to that appointment, my blood pressure was 140/90 so I was sent over to the hospital for an NST and then told to start a 24 hour urine when I got home. When I got to the hospital my blood pressure just kept going up. I think it was 160/110 at its highest. I was admitted. I was 24 weeks at that time. Luckily, my blood pressure stabilized but I was told that my baby and I were both sick and that I would likely be Care Flighted to a larger facility with a NICU. Instead, because my pressure had not spiked again on bedrest, I was sent home with a PE diagnosis and told to stay on strict bedrest.
I was scheduled for twice weekly NSTs and office visits. Each time I would go in for an NST my pressure would be sky high again, usually I’d be admitted and then sent home the next day. I think this repeated itself and then on the 5th admission I was told I would not be leaving until I delivered- whenever that would be. I was somewhere between 31-32 weeks. I developed gestational diabetes as well during this pregnancy and was taking insulin three times a day- the diabetes turned out to be a blessing later on because it had helped the baby to grow bigger than she otherwise would have been. I had daily NSTs, daily urine dips, weekly 24 hour urines, weekly growth scans, and weekly biophysical profiles. I kept asking to please be delivered but the doctor kept telling me the baby was “just too small.” Looking back and now having more understanding- being so small was every reason I should have been delivered.
Anyway, at 38 weeks, after 7 weeks of being in the hospital, the doctor finally agreed to deliver me IF an amnio proved the baby’s lungs were mature. That decision was made on a Saturday and the amnio was to be done on the following Monday. Monday morning came and they went to do the amnio and found that the baby’s fluid was virtually non-existent. They did not do the amnio and instead my induction was started 15 minutes later. I still believe that amnio saved my daughter’s life because if there had not been an amnio which showed the low fluid then my next ultrasound would not have been until Friday which I fear may have been too late. My labor was short and within about 3 hours I delivered a tiny 5 lb 15 oz baby girl.
We named her Anna. She had a very weak cry and a very thin cord but otherwise she seemed fine. I was started on a mag drip again and so the next 24 hours are very fuzzy. I do remember her having some grunting but was told over and over that she was fine. We were discharged home 2 days later and again I was not given any information about what could happen in the post partum period. Luckily during this pregnancy I found the Preeclampsia Foundation and so I knew. My blood pressure got far worse in the 6 weeks after birth than they ever were during the pregnancy. I was trialed on many medicines and I remain on lisinopril to this day. My blood pressure has not ever gone back to normal.
Due to my bedrest and not being able to work plus the mounting medical bills, we were financially devastated. Aside from trying to dig out from under that debt I thought the PE nightmare was over. Anna stayed very small and would not eat much. Even at about 3 months she was only taking 2 ounces of formula at a time. She vomited a lot also. The same doctor who had delivered her and who was our family doctor finally grew concerned enough that he sent us to pediatric GI specialist. We expected to go and be told we needed to concentrate her formula more and get something for her horrible projectile vomiting and reflux. My husband and I loaded Anna up and headed off to the appointment. We stopped and had lunch and the mood was so light. We finally got in to see the doctor and at that moment our lives were forever changed. He told us that he believed she had milk allergy and reflux and yes, she was tiny, but that he felt we had a much bigger problem. He felt like she had a neurological problem, likely cerebral palsy, and that we needed to get in to see a neurologist as soon as possible.
We left that appointment and drove home in complete silence. It took about a month to get in with the neurologist who confirmed the diagnosis. They feel her brain injury was suffered in utero from a lack of oxygen caused by a failing placenta. Her asymmetrical IUGR was proof of that. We immediately got her started in therapy and since that time have been to hell and back. She has had to endure countless specialists, appointments, a feeding tube, seizures, leg braces, medications… You name it and we’ve probably done it. She is an amazing child though and to look at her you would never know what all she has been through. The thing that is so hard is that her brain injury was preventable. Had my doctor not been so arrogant in thinking he could handle our case, her brain likely would have been spared. We should have been sent to an MFM or an OB at the very least. I have since found forgiveness for that doctor because the anger was making me crazy. I did not forgive for his sake, but for the sake of myself and my family. I firmly believe he did the best he knew how to do but sometimes doctors should admit they are in over their heads and ask for help. It wasn’t until I obtained all of our hospital records that I really realized how differently things should have gone.
Fast forward 3 more years and I became unexpectedly pregnant again. I found the best OB around who specializes in high risk pregnancies. He knew from the start that this pregnancy was going to be a balancing act and he was prepared for the job. He also understood how emotional this 9 months was going to be. I started bedrest at 20 weeks. I was on medication from the start and it was changed a few times. I had no idea how hard a pregnancy would be following a pregnancy that had gone wrong. The emotional toll was indescribable. But we made it successfully to 34 weeks when my pressures became unmanageable and I was induced. I delivered a 5 lb 13 oz little boy named Gabriel “Gabe”. He spent 18 days in the NICU before coming home. He is thriving and has healed a lot of the wounds that were so deep after my last pregnancy. For me, it was far easier to have a baby in the NICU that I knew was doing ok than to carry one inside of me that I could not see. I spent every day up until that day of delivery wondering if this baby’s brain would be ok and there was no test that could tell me the answer.
I was advised to never get pregnant again. I will listen to the doctors. I have learned to trust doctors again, but I have also learned to trust myself. I have learned to go with my gut instinct- the one that kept saying “get Anna delivered”, the one that I ignored. It has been a long road but one that has made me a better person. For us, the PE nightmare will never be over because the damage done to Anna’s brain cannot be undone. But we will go on and we will do our part to make sure this never happens to anyone else. All of my children are alive and so am I and because of that we are some of the lucky ones.
Jamie's Story
After about 1 ½ years of marriage my husband and I decided we were ready to have a baby. We were pregnant in no time and aside from the nausea and constant vomiting, I had a perfectly normal pregnancy until about 37 weeks. I thought I was going into labor and so I headed to labor and delivery to be checked out. I was not in labor, but my blood pressure was so high so I was kept overnight. I was sent home the next day on bedrest but went into labor that night and delivered a healthy 6 lb, 9 oz baby girl. We named her Carly. I was on the dreaded magnesium drip for 12 hours and then they turned it off. I was sent home without any instructions regarding what could happen after delivery... or that this same scenario could repeat itself in my next pregnancy.
Fast forward about 2 ½ years and we decided we were ready to give Carly a sibling. After a year of trying we were finally pregnant again. We live in a very small town and it is common here for people to use their family practice doctor as their OB. Since things had gone ok the first time I had no reason to believe things wouldn’t go the same way the second time. So off I went, back to my family practice doctor. Things were fairly routine again up until about 23 weeks. I was at work and started having contractions. I was very unconcerned at first and decided I just needed to drink some water and rest. I did but the contractions did not stop. I am an RN and worked at a hospital in a larger town about an hour away. It is important that I am a nurse because even with that education and experience I had no idea what could happen. I think we spent less than 30 minutes covering PE in nursing school and I worked in adult ICU and so we never deal with the women’s health side. In hindsight, I so wish I would have gone to labor and delivery where I worked instead of driving the hour home to go to the smaller hospital.
Oh hindsight is so very 20/20. Anyway, I drove home and went to L&D. At that time they did a fetal fibronectin test and noticed my pressures were a bit elevated. I was not seen by my doctor that day because he was not on call. The on call told me to go home on bedrest until the following Monday and then to follow up with my doctor for the test results. I did just as I was told. When I got to that appointment, my blood pressure was 140/90 so I was sent over to the hospital for an NST and then told to start a 24 hour urine when I got home. When I got to the hospital my blood pressure just kept going up. I think it was 160/110 at its highest. I was admitted. I was 24 weeks at that time. Luckily, my blood pressure stabilized but I was told that my baby and I were both sick and that I would likely be Care Flighted to a larger facility with a NICU. Instead, because my pressure had not spiked again on bedrest, I was sent home with a PE diagnosis and told to stay on strict bedrest.
I was scheduled for twice weekly NSTs and office visits. Each time I would go in for an NST my pressure would be sky high again, usually I’d be admitted and then sent home the next day. I think this repeated itself and then on the 5th admission I was told I would not be leaving until I delivered- whenever that would be. I was somewhere between 31-32 weeks. I developed gestational diabetes as well during this pregnancy and was taking insulin three times a day- the diabetes turned out to be a blessing later on because it had helped the baby to grow bigger than she otherwise would have been. I had daily NSTs, daily urine dips, weekly 24 hour urines, weekly growth scans, and weekly biophysical profiles. I kept asking to please be delivered but the doctor kept telling me the baby was “just too small.” Looking back and now having more understanding- being so small was every reason I should have been delivered.
Anyway, at 38 weeks, after 7 weeks of being in the hospital, the doctor finally agreed to deliver me IF an amnio proved the baby’s lungs were mature. That decision was made on a Saturday and the amnio was to be done on the following Monday. Monday morning came and they went to do the amnio and found that the baby’s fluid was virtually non-existent. They did not do the amnio and instead my induction was started 15 minutes later. I still believe that amnio saved my daughter’s life because if there had not been an amnio which showed the low fluid then my next ultrasound would not have been until Friday which I fear may have been too late. My labor was short and within about 3 hours I delivered a tiny 5 lb 15 oz baby girl.
We named her Anna. She had a very weak cry and a very thin cord but otherwise she seemed fine. I was started on a mag drip again and so the next 24 hours are very fuzzy. I do remember her having some grunting but was told over and over that she was fine. We were discharged home 2 days later and again I was not given any information about what could happen in the post partum period. Luckily during this pregnancy I found the Preeclampsia Foundation and so I knew. My blood pressure got far worse in the 6 weeks after birth than they ever were during the pregnancy. I was trialed on many medicines and I remain on lisinopril to this day. My blood pressure has not ever gone back to normal.
Due to my bedrest and not being able to work plus the mounting medical bills, we were financially devastated. Aside from trying to dig out from under that debt I thought the PE nightmare was over. Anna stayed very small and would not eat much. Even at about 3 months she was only taking 2 ounces of formula at a time. She vomited a lot also. The same doctor who had delivered her and who was our family doctor finally grew concerned enough that he sent us to pediatric GI specialist. We expected to go and be told we needed to concentrate her formula more and get something for her horrible projectile vomiting and reflux. My husband and I loaded Anna up and headed off to the appointment. We stopped and had lunch and the mood was so light. We finally got in to see the doctor and at that moment our lives were forever changed. He told us that he believed she had milk allergy and reflux and yes, she was tiny, but that he felt we had a much bigger problem. He felt like she had a neurological problem, likely cerebral palsy, and that we needed to get in to see a neurologist as soon as possible.
We left that appointment and drove home in complete silence. It took about a month to get in with the neurologist who confirmed the diagnosis. They feel her brain injury was suffered in utero from a lack of oxygen caused by a failing placenta. Her asymmetrical IUGR was proof of that. We immediately got her started in therapy and since that time have been to hell and back. She has had to endure countless specialists, appointments, a feeding tube, seizures, leg braces, medications… You name it and we’ve probably done it. She is an amazing child though and to look at her you would never know what all she has been through. The thing that is so hard is that her brain injury was preventable. Had my doctor not been so arrogant in thinking he could handle our case, her brain likely would have been spared. We should have been sent to an MFM or an OB at the very least. I have since found forgiveness for that doctor because the anger was making me crazy. I did not forgive for his sake, but for the sake of myself and my family. I firmly believe he did the best he knew how to do but sometimes doctors should admit they are in over their heads and ask for help. It wasn’t until I obtained all of our hospital records that I really realized how differently things should have gone.
Fast forward 3 more years and I became unexpectedly pregnant again. I found the best OB around who specializes in high risk pregnancies. He knew from the start that this pregnancy was going to be a balancing act and he was prepared for the job. He also understood how emotional this 9 months was going to be. I started bedrest at 20 weeks. I was on medication from the start and it was changed a few times. I had no idea how hard a pregnancy would be following a pregnancy that had gone wrong. The emotional toll was indescribable. But we made it successfully to 34 weeks when my pressures became unmanageable and I was induced. I delivered a 5 lb 13 oz little boy named Gabriel “Gabe”. He spent 18 days in the NICU before coming home. He is thriving and has healed a lot of the wounds that were so deep after my last pregnancy. For me, it was far easier to have a baby in the NICU that I knew was doing ok than to carry one inside of me that I could not see. I spent every day up until that day of delivery wondering if this baby’s brain would be ok and there was no test that could tell me the answer.
I was advised to never get pregnant again. I will listen to the doctors. I have learned to trust doctors again, but I have also learned to trust myself. I have learned to go with my gut instinct- the one that kept saying “get Anna delivered”, the one that I ignored. It has been a long road but one that has made me a better person. For us, the PE nightmare will never be over because the damage done to Anna’s brain cannot be undone. But we will go on and we will do our part to make sure this never happens to anyone else. All of my children are alive and so am I and because of that we are some of the lucky ones.
Wednesday, June 6, 2012
Bra Review II: Enell
 I'm sure you've been waiting with bated breath! Here is Bra Review Number Two: The Enell Bra. This was actually my first quality sports bra. Its claim to fame is being "Oprah's favorite sports bra". Since Oprah is a pretty curvy woman herself, it has to be good, right? Let's start with pros.
I'm sure you've been waiting with bated breath! Here is Bra Review Number Two: The Enell Bra. This was actually my first quality sports bra. Its claim to fame is being "Oprah's favorite sports bra". Since Oprah is a pretty curvy woman herself, it has to be good, right? Let's start with pros.
This is a monster of a bra. It is very durable. I've had one for over four years, and though it is a bit discolored, there's no other sign of wear. It will last practically forever.
This bra distributes the weight of the breasts across your whole back with a comfortable, wide back panel. The straps are wide and lightly padded, so no cutting into the shoulders. It's a fantastic compression bra, so there is no bounce. This is a very comfortable, supportive bra IF it fits you well.
And that brings us to the first con. It does not come in exact sizes; it comes in size ranges. It's basically a high quality small/medium/large type bra for curvy ladies. If you're between sizes, you're out of luck. Also, it clasps in the front with just one row of clasps. If you (like me) are the type to gain and lose the same five pounds over and over, you can't just move to a tighter or looser setting. The straps aren't adjustable, either, so if you're shorter or taller than average, you can't get a custom fit. I'm short, and I would prefer the straps to be just a bit shorter to really fit me well.
Now, the company does make custom bras. It costs an extra $15 for the first one, and once they have your pattern, it's an extra $7.50 for each additional bra.
The second big con for me is, again, it's a monster of a bra. It's very thick with no mesh parts. This makes it hot. I'm very heat sensitive when I run, as much as 2 min/mile slower in summer vs. winter. This is not my bra of choice for an outdoor long run if the weather is warmer than 30F/0C. I'm not kidding--my first winter of training, I often ran in a t-shirt with no gloves in 30-40F/0-4C weather with the Enell. (However, it was quite nice this past January the day I did 16 miles in 9F/-12C on snow and ice, but that's not typical weather most of the year.) Of course, since it's going to last forever, I'm not letting it go to waste. This has become my go-to bra when I run on the treadmill in the privacy of my home with no shirt and a fan pointed on me at all times.
So a mixed opinion. If it fits you well (or you're willing to pay the money for a custom bra) AND you don't mind the heat, it's a very comfortable bra that will last forever. But if it doesn't fit well and/or you're heat sensitive, look elsewhere. It gets a C- from me.
Note: I received no compensation for this review. This is just my opinion.
Note: I received no compensation for this review. This is just my opinion.
Saturday, June 2, 2012
Survivor Saturday: Sima's Story
I had the privilege of running 14 miles in honor of Sima and her children this morning. This story takes us from the tragedy of losing a child to the triumph of a successful second pregnancy. It also highlights a woman taking charge of her health and actively improving her risk status.
I just wanted to share my story to give hope to those who've lost a child to PE and are on their 2nd pregnancies. I lost my son seven years ago due to severe PE. He was born sleeping at just 500g (Severe IUGR) at 23weeks! My protein level if I remember correctly was 3++ and my BP was reading 190/95 or so. Having no knowledge of this condition, we were completely shocked and heart broken, the most traumatic incident to have happened to me and my husband.
After that we were so put off that we decided not to get pregnant for a while. I was on BP meds for at least a month after the delivery. The initial diagnosis was that I was obese and should lose the excess weight before going for a 2nd pregnancy. We decided then that we would just enjoy life and forget about having children for a while.
After a couple of years (still obese) one day I experienced severe headache. I went to my doctor, and she found that my BP was elevated 150/90, gave me some meds to get it down, and asked me to go home and rest. In the middle of the night I found my heart to be beating extremely fast. My husband and I decided to go in, and I was admitted. They performed an ECG / blood tests / 24 hr urine tests and found absolutely nothing. I was kept in for observation for a couple of days and was then told, as I was still young in my early 30's, that meds were not the right way to go, and that I must lose weight. I was then referred to a dietitian.
At the same time, I was asked to go in for an ultrasound of the kidneys just for reference. This is when we found out the 2nd shocking news that one of my kidneys was extremely small in size. No one could say if it was congenital or if it happened over a period of time. In any case, I was told by the doctor to definitely consider losing weight.
I lost around 18 kgs in a span of a year or so with lots of exercise and just a good diet. After that, we found that my BP levels had become normal. I was advised to have the small kidney removed if I could, as it was only functioning at 2% capacity. I had a laparoscopy to have that kidney removed.
We then consulted with the MFM to check to see whether we could try to get pregnant and were advised that all should be OK, and that I would be on LDA (low-dose aspirin) from as soon as the pregnancy is confirmed up to 34 weeks. I was advised conceiving with a single kidney was not a problem, either. While trying to get pregnant, I maintained a healthy diet and also worked out regularly.
And finally last year I became pregnant once again. I was very closely monitored by a good MFM throughout my pregnancy i.e. regular ultrasounds / doppler scans etc. There were no signs of any protein throughout the pregnancy, my BP level remained pretty steady i.e. within acceptable levels up until 24 weeks. Thereafter there was a slight increase, however more so due to anxiety and in some cases perhaps what is described as "white coat hypertension". The BP machine would beep whenever I was at the doctor's but absolutely fine when at home. I was asked to closely monitor my BP at home as well.
The anxiety levels were so high that my doctor asked me to find a means to relax and just think positive, as the pregnancy was going very smoothly. I did have quite a few braxton hicks plus a lot of acidity. I was also experiencing severe shoulder / arm aches on both sides during nights, which did cause a lot of nervousness, but after doctor's assurances that there was no way it would be what they call an epigastric pain, we relaxed a bit. Anything little that happened triggered us off, as the first time PE struck, it was very sudden with extremely high BP and proteinuria. I also had repeated UTI's but was told it was normal. The 1st time around the water retention in my feet was severe, this time around I was amazed to see that I could fit into my normal shoes.
I was asked to get myself admitted immediately if my home BP readings were anything higher than 140/90 and also if I experienced blurred vision or extreme water retention. During my pregnancy I was also doing yoga, though only up until week 16 as that's when my braxton hicks became quite painful so I was asked to stop. My pregnancy as per the doctors was basically pretty much uneventful (phewwww).
I was asked to come into the hospital on the first sign of labor pains. Come week 40 I was still hanging around waiting for the contractions. Since I was considered high risk, the doctors admitted me when I was 40 weeks 2 days. I was still not yet dilated and my cervix didn't seem ready at all even for an induction, so I opted for a C-section. I gave birth to a healthy baby girl at 40 weeks 4 days.
Words cannot describe our happiness! All the anxiety / nervousness etc. was worth it, as in the end we were blessed with a little bundle of joy. Though we waited over 6 years to conceive, it was well worth it. I believe my lifestyle change i.e. diet / exercise & weight loss also played a big part, though I firmly believe that obesity was NOT the cause of PE. In my case it was probably renal related as I had one small, improperly functioning kidney which was also the cause of repeated UTI's.
There is hope, ladies. We are now considering another baby, but the doctor thinks it's perhaps too risky as my bp levels after pregnancy have been slightly elevated, but then again only at the doctors. At home it's always fine. I have been asked to start taking hypertensives, but I think the better option would be to exercise and get back into shape as I did the last time, as it did help with my BP.
Sima's Story
I just wanted to share my story to give hope to those who've lost a child to PE and are on their 2nd pregnancies. I lost my son seven years ago due to severe PE. He was born sleeping at just 500g (Severe IUGR) at 23weeks! My protein level if I remember correctly was 3++ and my BP was reading 190/95 or so. Having no knowledge of this condition, we were completely shocked and heart broken, the most traumatic incident to have happened to me and my husband.
After that we were so put off that we decided not to get pregnant for a while. I was on BP meds for at least a month after the delivery. The initial diagnosis was that I was obese and should lose the excess weight before going for a 2nd pregnancy. We decided then that we would just enjoy life and forget about having children for a while.
After a couple of years (still obese) one day I experienced severe headache. I went to my doctor, and she found that my BP was elevated 150/90, gave me some meds to get it down, and asked me to go home and rest. In the middle of the night I found my heart to be beating extremely fast. My husband and I decided to go in, and I was admitted. They performed an ECG / blood tests / 24 hr urine tests and found absolutely nothing. I was kept in for observation for a couple of days and was then told, as I was still young in my early 30's, that meds were not the right way to go, and that I must lose weight. I was then referred to a dietitian.
At the same time, I was asked to go in for an ultrasound of the kidneys just for reference. This is when we found out the 2nd shocking news that one of my kidneys was extremely small in size. No one could say if it was congenital or if it happened over a period of time. In any case, I was told by the doctor to definitely consider losing weight.
I lost around 18 kgs in a span of a year or so with lots of exercise and just a good diet. After that, we found that my BP levels had become normal. I was advised to have the small kidney removed if I could, as it was only functioning at 2% capacity. I had a laparoscopy to have that kidney removed.
We then consulted with the MFM to check to see whether we could try to get pregnant and were advised that all should be OK, and that I would be on LDA (low-dose aspirin) from as soon as the pregnancy is confirmed up to 34 weeks. I was advised conceiving with a single kidney was not a problem, either. While trying to get pregnant, I maintained a healthy diet and also worked out regularly.
And finally last year I became pregnant once again. I was very closely monitored by a good MFM throughout my pregnancy i.e. regular ultrasounds / doppler scans etc. There were no signs of any protein throughout the pregnancy, my BP level remained pretty steady i.e. within acceptable levels up until 24 weeks. Thereafter there was a slight increase, however more so due to anxiety and in some cases perhaps what is described as "white coat hypertension". The BP machine would beep whenever I was at the doctor's but absolutely fine when at home. I was asked to closely monitor my BP at home as well.
The anxiety levels were so high that my doctor asked me to find a means to relax and just think positive, as the pregnancy was going very smoothly. I did have quite a few braxton hicks plus a lot of acidity. I was also experiencing severe shoulder / arm aches on both sides during nights, which did cause a lot of nervousness, but after doctor's assurances that there was no way it would be what they call an epigastric pain, we relaxed a bit. Anything little that happened triggered us off, as the first time PE struck, it was very sudden with extremely high BP and proteinuria. I also had repeated UTI's but was told it was normal. The 1st time around the water retention in my feet was severe, this time around I was amazed to see that I could fit into my normal shoes.
I was asked to get myself admitted immediately if my home BP readings were anything higher than 140/90 and also if I experienced blurred vision or extreme water retention. During my pregnancy I was also doing yoga, though only up until week 16 as that's when my braxton hicks became quite painful so I was asked to stop. My pregnancy as per the doctors was basically pretty much uneventful (phewwww).
I was asked to come into the hospital on the first sign of labor pains. Come week 40 I was still hanging around waiting for the contractions. Since I was considered high risk, the doctors admitted me when I was 40 weeks 2 days. I was still not yet dilated and my cervix didn't seem ready at all even for an induction, so I opted for a C-section. I gave birth to a healthy baby girl at 40 weeks 4 days.
Words cannot describe our happiness! All the anxiety / nervousness etc. was worth it, as in the end we were blessed with a little bundle of joy. Though we waited over 6 years to conceive, it was well worth it. I believe my lifestyle change i.e. diet / exercise & weight loss also played a big part, though I firmly believe that obesity was NOT the cause of PE. In my case it was probably renal related as I had one small, improperly functioning kidney which was also the cause of repeated UTI's.
There is hope, ladies. We are now considering another baby, but the doctor thinks it's perhaps too risky as my bp levels after pregnancy have been slightly elevated, but then again only at the doctors. At home it's always fine. I have been asked to start taking hypertensives, but I think the better option would be to exercise and get back into shape as I did the last time, as it did help with my BP.
Thursday, May 31, 2012
My Survivors
.jpg) |
| Smartie, 4 hours old, 10/2003 |
 |
| Smartie, 8.5 |
 |
| Sweetie, seconds old, 12/2006 |
 |
| Sweetie, 5.5 |
 |
| Monkey and Sassy, 1 day old, 7/2009 |
 |
| Monkey and Sassy, almost 3 |
Wednesday, May 30, 2012
An Intense Month of Posts
 |
| Almost done, ready to relax |
Preeclampsia Awareness Month is almost over. I'm almost done with my "Post a Day for the Month of May" challenge. It's been an intense month, but I'm glad to get information about PE and related conditions out there. I hope it is helpful to someone. One more post coming tomorrow, hopefully about the emotional impact of PE. (Just waiting for permission to reprint the article.) After that, I'll continue to post but not every day.
For more information and support, check out the Preeclampsia Foundation.
If you'd like to support my marathon fundraiser, click here.For more information and support, check out the Preeclampsia Foundation.
If you are looking for Survivor Stories, or have one to share, click here.
And an archive of the posts I've made:
On Preeclampsia:
Disclaimer
What Is Preeclampsia?
Why Me? (risk factors)
Trying Again After Preeclampsia
The Maternal-Fetal Conflict
A Nasty Little Protein
Risk Factors Revisited
On Treatment Options:
Bedrest
Exercise
Low Dose Aspirin
Vitamins and Minerals
The Brewer Diet
On the Emotional Impact:
The Aftermath
My Birth Burned Down
What Not To Say
A Fine Line (trigger warning: discusses death of a baby)
Other:
Observer's Bias
Tuesday, May 29, 2012
Treatment Options: The Brewer Diet
Disclaimer: I am not a doctor. This is provided for information only. Please consult your health care provider before starting or stopping a treatment plan.
The Brewer Diet, created by Dr. Tom Brewer starting in the 1960s, claims to be a 100% prevention/cure for preeclampsia. This diet is very popular in the natural birth community. After all, what could be more natural than eating healthy? But how does this diet stand up to research? Does it live up to its claim to prevent PE?
In the 1960s, common obstetric practices and treatments for PE involved many things we now know are harmful, things Dr. Brewer spoke out against. He was correct about those poor practices. He also was correct that eating a quality diet during pregnancy is important for the health of both mother and child. I give him credit for that.
Dr. Brewer believed PE was entirely due to poor nutrition, in particular a lack of dietary protein. In fact, he was so convinced of the role of nutrition in the development of PE, he renamed the condition Metabolic Toxemia of Late Pregnancy, or MTLP.
After spending a number of hours over several days reading the primary websites dedicated to the Brewer diet, I still have little understanding of his basic theory. The gist of it is that the body needs protein to increase blood volume enough to sustain a pregnancy. Without adequate dietary intake, blood volume cannot keep up with the demands of the pregnancy, triggering the cascade of symptoms. How he believed this happens, it is not clear. His own research was not peer-reviewed, and I can find no outside research to support this theory, either in his website's own bibliography or in a search of PubMed.
Considering Dr. Brewer claimed a 100% success rate, it would be reasonable to ask, has any woman followed the Brewer Diet and gotten PE anyway? A search of the Preeclampsia Foundation's forums quickly shows there are many women who have, some of them quite severely. But according to this website, the answer is no, there has never been a woman who *correctly* followed the Brewer Diet and got sick anyway. There are only women who *think* they were following the diet, but they couldn't possibly have followed it correctly. Therefore, their experiences do not count as a failure of the diet.
Dr. Brewer himself said in his Aphorism No. 5, "The well-fed, well-salted, well-watered, NON-DRUGGED pregnant lady often develops water retention ("edema" or "oedema") and blood pressure rise (”hypertension”) and protein in her urine ("albuminuria") and "excessive weight gain" which are mistakenly diagnosed as "pre-eclampsia."" In other words, if a woman who is not on his diet has these symptoms, she has PE, but if she has the exact same symptoms while on his diet, it's just a normal part of pregnancy? Um, no. It's PE, and it's dangerous, even more so because a woman might not get the treatment she desperately needs because she's been told her symptoms are normal.
Then there's this claim of "mistaken diagnosis." If a woman has symptoms of PE but is well-nourished to Dr. Brewer's standards, it must not be PE but rather another condition that causes the same symptoms. Um, a condition exactly like PE? That causes the exact same symptoms? But NOT PE? Because, again, it couldn't be the diet that failed. It must be this mysterious Not-PE condition. Hm, could this be a case of Observer's Bias?
(Might I point out that ANY treatment plan can claim a 100% success rate if one simply refuses to acknowledge the failures.)
Another good question to ask would be, has any woman NOT followed the Brewer Diet and NOT gotten PE? And the answer is of course! Every year around the world, hundreds of millions of pregnant women eat a diet that does not meet Dr. Brewer's standards, yet without getting PE. This can range from women in America who eat processed junk and fast food, to women in famine-stricken Africa who do not get enough calories, period, let alone 100g of protein, to vegans who eat a generally healthy diet overall but not quite "perfect". Why do these women NOT get PE when women who followed (or "thought they were following") the Brewer diet do? Clearly, there must be more to it than diet alone. But once you acknowledge that something else can be in play, Dr. Brewer's theories fall apart.
Oh, but maybe it's similar to Type II Diabetes. One must have a predisposition for the condition. If you don't have that predisposition, you can eat whatever crap you want and be fine regardless, but if you DO have the predisposition, you must be very careful about what you eat. If this were true, you would expect to find that women with the worst diets have the highest rates and most severe cases of PE, while those who have generally good (but not quite perfect) diets would have the fewest and mildest cases. But the largest US study on PE and diet ever done (looking specifically at calcium, not protein, but with detailed diet evaluations of all participants) found no difference in the protein intake among those who did and did not get PE, nor did they find any difference in the PE rates among women with poor, fair, and good diets.
But Dr. Brewer was right about those bad obstetric practices back in the '60s. And he was right that traditional treatments for hypertension, in particular salt restricion, wouldn't help (because hypertension is merely a symptom, not the primary problem). So why couldn't his diet theory also be correct?
Considering what we now know about the role of sFlt1 in the cascade of symptoms, his dietary protein theory just doesn't make sense. Oh, but there's an answer for that, too. Just because all women with PE have elevated sFlt1 and no woman without PE has elevated sFlt1, that doesn't mean sFlt1 has anything to do with causing PE. No, if anything it was poor diet that caused the elevated sFlt1, even though women without PE who eat a poor diet don't have elevated sFlt1, and women with a good diet and PE do. I've said it before, I'll say it again: Observer's Bias.
Oh, but what about all the women who follow the Brewer Diet and don't get PE? Who are true believers that it helped them? Well, 90% of women will never get PE whether they follow the diet or not. It doesn't mean the diet saved them. But what about women who got PE the first time around, then discovered and followed the diet, and didn't get PE the second time around? Again, most women who get PE only get it once. This anecdotal "data" doesn't prove it works.
Can I say with certainty that the Brewer Diet doesn't work at all? No, I can't. PE is a very complex condition, and we have a long way to go to unravel all the risk factors that go into it. There may be some women out there for whom the Brewer Diet can make the difference. But it DOES NOT live up to its claim of 100% prevention/cure. It merely ignores failures as either "normal", "misdiagnosed", or a failure of the woman who "didn't follow it correctly".
The Brewer Diet, created by Dr. Tom Brewer starting in the 1960s, claims to be a 100% prevention/cure for preeclampsia. This diet is very popular in the natural birth community. After all, what could be more natural than eating healthy? But how does this diet stand up to research? Does it live up to its claim to prevent PE?
In the 1960s, common obstetric practices and treatments for PE involved many things we now know are harmful, things Dr. Brewer spoke out against. He was correct about those poor practices. He also was correct that eating a quality diet during pregnancy is important for the health of both mother and child. I give him credit for that.
Dr. Brewer believed PE was entirely due to poor nutrition, in particular a lack of dietary protein. In fact, he was so convinced of the role of nutrition in the development of PE, he renamed the condition Metabolic Toxemia of Late Pregnancy, or MTLP.
After spending a number of hours over several days reading the primary websites dedicated to the Brewer diet, I still have little understanding of his basic theory. The gist of it is that the body needs protein to increase blood volume enough to sustain a pregnancy. Without adequate dietary intake, blood volume cannot keep up with the demands of the pregnancy, triggering the cascade of symptoms. How he believed this happens, it is not clear. His own research was not peer-reviewed, and I can find no outside research to support this theory, either in his website's own bibliography or in a search of PubMed.
Considering Dr. Brewer claimed a 100% success rate, it would be reasonable to ask, has any woman followed the Brewer Diet and gotten PE anyway? A search of the Preeclampsia Foundation's forums quickly shows there are many women who have, some of them quite severely. But according to this website, the answer is no, there has never been a woman who *correctly* followed the Brewer Diet and got sick anyway. There are only women who *think* they were following the diet, but they couldn't possibly have followed it correctly. Therefore, their experiences do not count as a failure of the diet.
Dr. Brewer himself said in his Aphorism No. 5, "The well-fed, well-salted, well-watered, NON-DRUGGED pregnant lady often develops water retention ("edema" or "oedema") and blood pressure rise (”hypertension”) and protein in her urine ("albuminuria") and "excessive weight gain" which are mistakenly diagnosed as "pre-eclampsia."" In other words, if a woman who is not on his diet has these symptoms, she has PE, but if she has the exact same symptoms while on his diet, it's just a normal part of pregnancy? Um, no. It's PE, and it's dangerous, even more so because a woman might not get the treatment she desperately needs because she's been told her symptoms are normal.
Then there's this claim of "mistaken diagnosis." If a woman has symptoms of PE but is well-nourished to Dr. Brewer's standards, it must not be PE but rather another condition that causes the same symptoms. Um, a condition exactly like PE? That causes the exact same symptoms? But NOT PE? Because, again, it couldn't be the diet that failed. It must be this mysterious Not-PE condition. Hm, could this be a case of Observer's Bias?
(Might I point out that ANY treatment plan can claim a 100% success rate if one simply refuses to acknowledge the failures.)
Another good question to ask would be, has any woman NOT followed the Brewer Diet and NOT gotten PE? And the answer is of course! Every year around the world, hundreds of millions of pregnant women eat a diet that does not meet Dr. Brewer's standards, yet without getting PE. This can range from women in America who eat processed junk and fast food, to women in famine-stricken Africa who do not get enough calories, period, let alone 100g of protein, to vegans who eat a generally healthy diet overall but not quite "perfect". Why do these women NOT get PE when women who followed (or "thought they were following") the Brewer diet do? Clearly, there must be more to it than diet alone. But once you acknowledge that something else can be in play, Dr. Brewer's theories fall apart.
Oh, but maybe it's similar to Type II Diabetes. One must have a predisposition for the condition. If you don't have that predisposition, you can eat whatever crap you want and be fine regardless, but if you DO have the predisposition, you must be very careful about what you eat. If this were true, you would expect to find that women with the worst diets have the highest rates and most severe cases of PE, while those who have generally good (but not quite perfect) diets would have the fewest and mildest cases. But the largest US study on PE and diet ever done (looking specifically at calcium, not protein, but with detailed diet evaluations of all participants) found no difference in the protein intake among those who did and did not get PE, nor did they find any difference in the PE rates among women with poor, fair, and good diets.
But Dr. Brewer was right about those bad obstetric practices back in the '60s. And he was right that traditional treatments for hypertension, in particular salt restricion, wouldn't help (because hypertension is merely a symptom, not the primary problem). So why couldn't his diet theory also be correct?
Considering what we now know about the role of sFlt1 in the cascade of symptoms, his dietary protein theory just doesn't make sense. Oh, but there's an answer for that, too. Just because all women with PE have elevated sFlt1 and no woman without PE has elevated sFlt1, that doesn't mean sFlt1 has anything to do with causing PE. No, if anything it was poor diet that caused the elevated sFlt1, even though women without PE who eat a poor diet don't have elevated sFlt1, and women with a good diet and PE do. I've said it before, I'll say it again: Observer's Bias.
Oh, but what about all the women who follow the Brewer Diet and don't get PE? Who are true believers that it helped them? Well, 90% of women will never get PE whether they follow the diet or not. It doesn't mean the diet saved them. But what about women who got PE the first time around, then discovered and followed the diet, and didn't get PE the second time around? Again, most women who get PE only get it once. This anecdotal "data" doesn't prove it works.
Can I say with certainty that the Brewer Diet doesn't work at all? No, I can't. PE is a very complex condition, and we have a long way to go to unravel all the risk factors that go into it. There may be some women out there for whom the Brewer Diet can make the difference. But it DOES NOT live up to its claim of 100% prevention/cure. It merely ignores failures as either "normal", "misdiagnosed", or a failure of the woman who "didn't follow it correctly".
Monday, May 28, 2012
Treatment Options: Vitamins and Minerals
Disclaimer: I am not a doctor. This is provided for informational purposes only. As always, consult your health care provider before starting or stopping a treatment plan.
Diet is such a complex issue. I plan to cover it in several posts. Today's post focuses on vitamins and minerals.
 We all know how important it is to eat healthy, and especially during pregnancy. We all know we should be eating whole foods with lots of fresh fruits and vegetables, whole grains, lean meats, and healthy fats. We know we should not be eating processed foods or lots of sugar or refined grains. Eating well will keep you and your baby as healthy as possible so you both have the best chance of surviving any complication that may come up, including preelcampsia and related conditions. But will diet prevent PE?
We all know how important it is to eat healthy, and especially during pregnancy. We all know we should be eating whole foods with lots of fresh fruits and vegetables, whole grains, lean meats, and healthy fats. We know we should not be eating processed foods or lots of sugar or refined grains. Eating well will keep you and your baby as healthy as possible so you both have the best chance of surviving any complication that may come up, including preelcampsia and related conditions. But will diet prevent PE?
This 2008 study looked at the blood work of women who already had preeclampsia and compared it to both healthy pregnant women and non-pregnant women. It found women with PE had lower levels of antioxidant enzymes and vitamins A, D, and E. This shows there is a connection to nutrients in the blood and preeclampsia. But the question remains: did deficiencies cause PE, did PE cause deficiencies, or is there some other factor at play in both of these? More importantly, would correcting these deficiencies prevent PE?
This recent review looked at taking antioxidant supplements as a way to prevent PE. It found no improvement in outcomes. This 2008 review actually found an increase in pregnancy induced hypertention with antioxidant supplements, although it did not appear that these cases progressed to full PE any more often.
This review looked at vitamin E supplementation. It showed mixed results--when analyzed one way, the data showed decreased PE rates, but another way showed no change. A similar mixed result of data occured in this review looking at supplementing vitamin C. It did show increased risk of preterm birth with vitamin C supplementation.
This article reported that many pregnant women are deficient in vitamin D. Not all women who are deficient develop PE, and not all women who develop PE are deficient, but a greater percentage of women with PE are deficient than those without PE. So it appears vitamin D deficiency raises risk of PE, but it's not an absolute connection. This review found that supplementing women deficient in vitamin D did raise the levels in their blood, but that did not change the rates of PE.
This study found calcium deficiencies in blood work of severely preeclamptic women compared to healthy pregnant women. This large study attempted to prevent PE through calcium supplementation. The results were no difference in PE rates among the supplemented and placebo groups.
From the above studies, it appears improving intake of various vitamins and minerals offers little to no benefit in the prevention of preeclampsia. Yes, we should definitely be eating healthy. But we can't count on diet to prevent PE.
Diet is such a complex issue. I plan to cover it in several posts. Today's post focuses on vitamins and minerals.
 We all know how important it is to eat healthy, and especially during pregnancy. We all know we should be eating whole foods with lots of fresh fruits and vegetables, whole grains, lean meats, and healthy fats. We know we should not be eating processed foods or lots of sugar or refined grains. Eating well will keep you and your baby as healthy as possible so you both have the best chance of surviving any complication that may come up, including preelcampsia and related conditions. But will diet prevent PE?
We all know how important it is to eat healthy, and especially during pregnancy. We all know we should be eating whole foods with lots of fresh fruits and vegetables, whole grains, lean meats, and healthy fats. We know we should not be eating processed foods or lots of sugar or refined grains. Eating well will keep you and your baby as healthy as possible so you both have the best chance of surviving any complication that may come up, including preelcampsia and related conditions. But will diet prevent PE? This 2008 study looked at the blood work of women who already had preeclampsia and compared it to both healthy pregnant women and non-pregnant women. It found women with PE had lower levels of antioxidant enzymes and vitamins A, D, and E. This shows there is a connection to nutrients in the blood and preeclampsia. But the question remains: did deficiencies cause PE, did PE cause deficiencies, or is there some other factor at play in both of these? More importantly, would correcting these deficiencies prevent PE?
This recent review looked at taking antioxidant supplements as a way to prevent PE. It found no improvement in outcomes. This 2008 review actually found an increase in pregnancy induced hypertention with antioxidant supplements, although it did not appear that these cases progressed to full PE any more often.
This review looked at vitamin E supplementation. It showed mixed results--when analyzed one way, the data showed decreased PE rates, but another way showed no change. A similar mixed result of data occured in this review looking at supplementing vitamin C. It did show increased risk of preterm birth with vitamin C supplementation.
This article reported that many pregnant women are deficient in vitamin D. Not all women who are deficient develop PE, and not all women who develop PE are deficient, but a greater percentage of women with PE are deficient than those without PE. So it appears vitamin D deficiency raises risk of PE, but it's not an absolute connection. This review found that supplementing women deficient in vitamin D did raise the levels in their blood, but that did not change the rates of PE.
This study found calcium deficiencies in blood work of severely preeclamptic women compared to healthy pregnant women. This large study attempted to prevent PE through calcium supplementation. The results were no difference in PE rates among the supplemented and placebo groups.
From the above studies, it appears improving intake of various vitamins and minerals offers little to no benefit in the prevention of preeclampsia. Yes, we should definitely be eating healthy. But we can't count on diet to prevent PE.
Sunday, May 27, 2012
Treatment Options: Low-Dose Aspirin
Disclaimer: I am not a doctor. This is provided for information only. Please consult your health care provider to discuss the treatment option(s) that are right for your specific case.
So far we've discussed bedrest and exercise. I'm still working on nutrition, which will be covered in several posts this week. Today I want to focus on low-dose aspirin and other anticoagulants.
Preeclampsia is associated with changes in the way a woman's blood clots. One theory that has emerged is that blood thinners could counteract these changes and prevent PE. Several studies were done on aspirin in pregnancy during the 1980s and 1990s.
This review of multiple studies, explained in more understandable terms in this article, did find a small but real reduction in preeclampsia rates when women at high risk took low-dose aspirin. It is important to note that it doesn't help everyone. So far, researchers have not found a way to determine which high-risk women will benefit and which will not. This study found further reduction of risk (though still not large) when low-dose aspirin was paired with low molecular weight heparin, a prescription blood thinner.
This article points out there are risks involved with low-dose aspirin as well, although those risks are small, and questions whether it is worth giving it to so many women who won't benefit from it just to save the few who do.
Aspirin therapy is not currently recommended to the general population of pregnant women, but for those who have a history of severe PE and/or have multiple risk factors, it is worth discussing with your doctor if it is a reasonable option.
So far we've discussed bedrest and exercise. I'm still working on nutrition, which will be covered in several posts this week. Today I want to focus on low-dose aspirin and other anticoagulants.
Preeclampsia is associated with changes in the way a woman's blood clots. One theory that has emerged is that blood thinners could counteract these changes and prevent PE. Several studies were done on aspirin in pregnancy during the 1980s and 1990s.
This review of multiple studies, explained in more understandable terms in this article, did find a small but real reduction in preeclampsia rates when women at high risk took low-dose aspirin. It is important to note that it doesn't help everyone. So far, researchers have not found a way to determine which high-risk women will benefit and which will not. This study found further reduction of risk (though still not large) when low-dose aspirin was paired with low molecular weight heparin, a prescription blood thinner.
This article points out there are risks involved with low-dose aspirin as well, although those risks are small, and questions whether it is worth giving it to so many women who won't benefit from it just to save the few who do.
Aspirin therapy is not currently recommended to the general population of pregnant women, but for those who have a history of severe PE and/or have multiple risk factors, it is worth discussing with your doctor if it is a reasonable option.
Saturday, May 26, 2012
Survivor Saturday: Tracy's Story
I ran 10 miles in honor of Tracy and her children today. Tracy had hypertension outside pregnancy and a family history. She developed PE post partum. This story highlights the lingering emotional effects of a high risk pregnancy and traumatic birth.
I am chronically hypertensive and have been most of my life. That and the fact that my mother developed preeclampsia while pregnant with me and had to be induced made me "high risk" for preeclampsia. I was already on medication for my high blood pressure when I became pregnant with my first child, and my pregnancy was overseen by my family practice doctor who consulted with a perinatologist who specializes in hypertension in pregnancy. The perinatologist added more medications and, halfway through my pregnancy, as my blood pressure began to rise, he took over management of my pregnancy. As my pregnancy progressed, I began to feel less and less in control of how things would develop. At one appointment, I recall the doctor telling me that I would be having an epidural during my labour to help control my blood pressure. I had been hoping to avoid an epidural. But I was young, this was my first pregnancy and I didn't really have any other sources of information back then. The internet was not nearly the resource of information 15 years ago as it is today!
At around 28 weeks or so, as my blood pressure began to rise, the doctor had me coming in 3 to 4 times a week for fetal monitoring and to have my blood pressure checked. At 31 weeks, while being monitored on the L&D ward, the nurse took my blood pressure and it had sky-rocketed. The doctor admitted me and started to add and change medications while keeping me on continuous blood pressure monitoring and frequent fetal monitoring. I was prepared for the possibility that the baby might have to be delivered prematurely and, after a few days in hospital, when my blood pressure had appeared to stabilize, I was able to tour the NICU. I was in hospital for a week when the doctor was satisfied that the medications were working and the baby was still doing well. I was sent home on strict bed rest for the rest of the pregnancy and told that, if I made it that far, I would be induced at 37 weeks. I'll never forget sitting in the doctor's office during a follow up appointment and watching as Dr. E. pulled a little black notebook from his coat pocket and penciled in my baby's birthday.
For five more weeks, I returned to the hospital 3 or 4 times a week for fetal monitoring and spent the rest of the time on bed rest. Between late pregnancy, high blood pressure and weeks of bed rest, I found I could barely shower without completely wearing myself out. I was growing crazy in the house but was too worn out even for guests when they visited. A week before I was to be induced, I underwent a miserable amniocentisis to determine the baby's lung maturity. Then, I was told to report to L&D at 36 weeks and 5 days, to check in and prepare for being induced the next day.
We checked into L&D at the appointed time and I was offered the suite with a whirl pool as it was available. I turned it down, under the impression I wouldn't be able to use it, which I later regretted. I mightn't have been able to use it, I don't know, but it might have helped if I could have. A prostoglandin gel was applied to my cervix, DH and I had some dinner, watched some television and then went to sleep. Along with my meds, I was given a sleeping pill which was lovely. Probably the most (only!) enjoyable part of my hospital stay!
As expected, the prostoglandin gel had had little effect on my cervix by the next morning and a pitocin drip was started to get labour going. The contractions weren't too intense for the next couple of hours and I recall DH and I just chatting with each other and staff that wandered in and out, watching the read out on the fetal monitor and watching for contractions.
Most of the labour is a blur to me now as it was so long ago. I recall the contractions becoming worse as the day progressed and trying a warm shower, which didn't help too much. Finally, I got some pain relief (Demoral, I think?) which really didn't help much at all. I remember feeling like my entire abdomen was on fire and, as I was trapped in bed on the monitor, I couldn't do much about it. At one point, the baby's heart rate dipped very low and they put me on oxygen for the rest of the labour. An epidural was ordered but I had to wait for what seemed like an eternity before the anesthesiologist finally came. The epidural managed to numb all of my pain except for the lower right quadrant, which continued to feel as if it were on fire. I was exhausted and, once the epidural had kicked in (well, mostly) I started to drift in and out of sleep.
At around 4 AM I was told it was time to push. I remember feeling completely confused. Push how? Where? With what? I couldn't feel anything and had no idea what I was supposed to be pushing or what to push with. It was bizarre. Just before the pushing began, however, the epidural had begun to wear off and the pain had started return. At first, I just did what I thought they were telling me to do with no idea whatsoever if I was actually doing anything. I couldn't feel it. But as the feeling came back, the pushing started to feel almost involuntary. I remember everyone counting and instructing me when to push and how long. I couldn't push for as long as they wanted. It felt all wrong and I thought I was doing it all wrong because I didn't know what I was doing.
After nearly 39 minutes of pushing, the baby was no longer descending and they noticed that every time I pushed, her heart rate dropped down way too low. They told me to stop pushing and I recall the room suddenly filling with people. No one told me anything was wrong but I knew something was happening when the room suddenly filled like that. From what I could later tell, the cord was wrapped too tightly around the baby's neck to allow her to descend any further and every time I pushed, the circulation in the umbilical cord was cut off which caused her heart rate to plummet. An episiotomy was cut and forceps were brought out. I was already in horrible pain and the pain of the forcep delivery was indescribable. The baby's head was delivered, the cord clamped and cut, and then the rest of her was born. I didn't get to see her face. The first glimpse I had of her was of two tiny purple buns as they whisked her away to a warming table to examine her. I don't think she cried right away. They were concerned with her breathing and told us they would be taking her to NICU for observation. DH told them he'd like for me to see her first before they took her away and they wrapped her up and put her in my arms. I was able to hold her for a few minutes, then she was taken to NICU. I sent DH with her.
After a period of time, Tory was brought back from NICU by a nurse who announced "there's nothing wrong with this baby, she doesn't need to be in NICU!" Another nurse then bathed her and dressed her in the little white preemie outfit we'd brought with us to the hospital. Shortly after, a photographer came in to take her first portrait and then we were moved to the maternity ward.
We were released to go home on Tuesday. I was on a number of drugs for my blood pressure and lasix for the water retention (which did nothing to help establish my milk supply, sadly) and we were told to have Tory's bilirubin levels checked at Children's hospital every other day. We took Tory to have her bilirubin levels checked on Wednesday and Thursday and on Friday morning, a nurse came to our home to set up a special bili light unit which Tory was to stay under for the next day and a half or so. We had to leave her under the lights except to feed her and she was also wrapped in a little "glow worn" vest around her middle. Breastfeeding was not going well, both DH and I were overwhelmed and exhausted, we were supplementing with bottles of formula and the heat was oppressive. I was feeling increasingly worse, but put it down to the heat and exhaustion.
On Sunday, Tory was finished with the bili lights and we gave her a bath. We'd been in the house all week and we decided to go shopping. We pulled ourselves together, packed Tory up and headed to the local mall. We'd been walking around in a drugstore for a little while when I started feeling very strange. It's hard to explain, but I just didn't feel right. We went home and DH checked my blood pressure. It had spiked really high. We waited a bit to see if it came back down with some rest, but it didn't. DH called the hospital and we were told to come in.
At the hospital, my blood pressure was still very high and they did some labs and determined I had developed preeclampsia. I was admitted and started on mag sulfate. I hated the mag. It made me feel like I was going to come right out of my skin. I felt completely out of it and so foggy I couldn't even carry on a conversation, but my body was so restless and uncomfortable, I thought I didn't know what to do with myself. I started to panic that Tory would be hungry by now but I just couldn't nurse her. I couldn't even hold her. I watched as DH gave her a bottle and felt awful. She was getting too many bottles and too much formula and I felt so defeated. I couldn't stand the restlessness anymore and finally complained. I was given something to help with the restlessness, perhaps a sedative, I don't remember anymore, and it helped. I think I slept. It was Sunday evening, one week to the day since Tory was born, and here I was back in the hospital. I spent the first few days in and out of it, I think because I was just so exhausted. Tory stayed with me and DH was also able to stay and care for her. I felt resentful that I had developed preeclampsia in spite of the fact that Tory's birth had been induced to avoid this very thing. I wondered if we could have just let her birth come spontaneously, since the induction hadn't prevented preeclampsia anyway. Later, someone remarked "Wow, it's a good thing you were induced before the preeclampsia developed!" I hadn't thought of it that way. But they were right. At least, my preeclampsia didn't involve my baby.
I was in hospital for a week and sent home with new medications. In the weeks and months that followed, DH returned to work and I continued to struggle to breastfeed Tory and get sleep where I could. I was still exhausted and I was very disappointed how Tory's birth and first weeks had unfolded. I started to lose interest in everything and had decided I was an awful mother. I told DH I wanted him to stay home and care for Tory and I would go to work. When I saw pregnant women, I honestly pitied them. I swore we would never have another child and was so convinced of this that I felt guilty and sorry for Tory that she would be raised an only child. I became so miserable that I felt like I was moving through a thick fog and only looked forward to when Tory was someday start college and all this struggle to breastfeed, the sleepless nights, and the guilt and disappointment over her birth would be far behind me. When Tory was about 3 months old, I was diagnosed with severe PPD and started medication and therapy. It made all the difference and I started to feel like a human being again. Even happy. Things improved steadily after that.
My experience with preeclampsia has put a cloud of fear over each of my subsequent pregnancies. I've tried baby aspirin therapy, vitamin C and E therapy, the Brewer diet and I can't remember what else. I've had problems with my blood pressure with each of my pregnancies, but thankfully have not had a repeat of preeclampsia. And, of course, I worry for when my daughters become pregnant some day. I hope, by that time, we will understand preeclampsia better and be able to prevent it completely.
Tracy's Story
I am chronically hypertensive and have been most of my life. That and the fact that my mother developed preeclampsia while pregnant with me and had to be induced made me "high risk" for preeclampsia. I was already on medication for my high blood pressure when I became pregnant with my first child, and my pregnancy was overseen by my family practice doctor who consulted with a perinatologist who specializes in hypertension in pregnancy. The perinatologist added more medications and, halfway through my pregnancy, as my blood pressure began to rise, he took over management of my pregnancy. As my pregnancy progressed, I began to feel less and less in control of how things would develop. At one appointment, I recall the doctor telling me that I would be having an epidural during my labour to help control my blood pressure. I had been hoping to avoid an epidural. But I was young, this was my first pregnancy and I didn't really have any other sources of information back then. The internet was not nearly the resource of information 15 years ago as it is today!
At around 28 weeks or so, as my blood pressure began to rise, the doctor had me coming in 3 to 4 times a week for fetal monitoring and to have my blood pressure checked. At 31 weeks, while being monitored on the L&D ward, the nurse took my blood pressure and it had sky-rocketed. The doctor admitted me and started to add and change medications while keeping me on continuous blood pressure monitoring and frequent fetal monitoring. I was prepared for the possibility that the baby might have to be delivered prematurely and, after a few days in hospital, when my blood pressure had appeared to stabilize, I was able to tour the NICU. I was in hospital for a week when the doctor was satisfied that the medications were working and the baby was still doing well. I was sent home on strict bed rest for the rest of the pregnancy and told that, if I made it that far, I would be induced at 37 weeks. I'll never forget sitting in the doctor's office during a follow up appointment and watching as Dr. E. pulled a little black notebook from his coat pocket and penciled in my baby's birthday.
For five more weeks, I returned to the hospital 3 or 4 times a week for fetal monitoring and spent the rest of the time on bed rest. Between late pregnancy, high blood pressure and weeks of bed rest, I found I could barely shower without completely wearing myself out. I was growing crazy in the house but was too worn out even for guests when they visited. A week before I was to be induced, I underwent a miserable amniocentisis to determine the baby's lung maturity. Then, I was told to report to L&D at 36 weeks and 5 days, to check in and prepare for being induced the next day.
We checked into L&D at the appointed time and I was offered the suite with a whirl pool as it was available. I turned it down, under the impression I wouldn't be able to use it, which I later regretted. I mightn't have been able to use it, I don't know, but it might have helped if I could have. A prostoglandin gel was applied to my cervix, DH and I had some dinner, watched some television and then went to sleep. Along with my meds, I was given a sleeping pill which was lovely. Probably the most (only!) enjoyable part of my hospital stay!
As expected, the prostoglandin gel had had little effect on my cervix by the next morning and a pitocin drip was started to get labour going. The contractions weren't too intense for the next couple of hours and I recall DH and I just chatting with each other and staff that wandered in and out, watching the read out on the fetal monitor and watching for contractions.
Most of the labour is a blur to me now as it was so long ago. I recall the contractions becoming worse as the day progressed and trying a warm shower, which didn't help too much. Finally, I got some pain relief (Demoral, I think?) which really didn't help much at all. I remember feeling like my entire abdomen was on fire and, as I was trapped in bed on the monitor, I couldn't do much about it. At one point, the baby's heart rate dipped very low and they put me on oxygen for the rest of the labour. An epidural was ordered but I had to wait for what seemed like an eternity before the anesthesiologist finally came. The epidural managed to numb all of my pain except for the lower right quadrant, which continued to feel as if it were on fire. I was exhausted and, once the epidural had kicked in (well, mostly) I started to drift in and out of sleep.
At around 4 AM I was told it was time to push. I remember feeling completely confused. Push how? Where? With what? I couldn't feel anything and had no idea what I was supposed to be pushing or what to push with. It was bizarre. Just before the pushing began, however, the epidural had begun to wear off and the pain had started return. At first, I just did what I thought they were telling me to do with no idea whatsoever if I was actually doing anything. I couldn't feel it. But as the feeling came back, the pushing started to feel almost involuntary. I remember everyone counting and instructing me when to push and how long. I couldn't push for as long as they wanted. It felt all wrong and I thought I was doing it all wrong because I didn't know what I was doing.
After nearly 39 minutes of pushing, the baby was no longer descending and they noticed that every time I pushed, her heart rate dropped down way too low. They told me to stop pushing and I recall the room suddenly filling with people. No one told me anything was wrong but I knew something was happening when the room suddenly filled like that. From what I could later tell, the cord was wrapped too tightly around the baby's neck to allow her to descend any further and every time I pushed, the circulation in the umbilical cord was cut off which caused her heart rate to plummet. An episiotomy was cut and forceps were brought out. I was already in horrible pain and the pain of the forcep delivery was indescribable. The baby's head was delivered, the cord clamped and cut, and then the rest of her was born. I didn't get to see her face. The first glimpse I had of her was of two tiny purple buns as they whisked her away to a warming table to examine her. I don't think she cried right away. They were concerned with her breathing and told us they would be taking her to NICU for observation. DH told them he'd like for me to see her first before they took her away and they wrapped her up and put her in my arms. I was able to hold her for a few minutes, then she was taken to NICU. I sent DH with her.
After a period of time, Tory was brought back from NICU by a nurse who announced "there's nothing wrong with this baby, she doesn't need to be in NICU!" Another nurse then bathed her and dressed her in the little white preemie outfit we'd brought with us to the hospital. Shortly after, a photographer came in to take her first portrait and then we were moved to the maternity ward.
We were released to go home on Tuesday. I was on a number of drugs for my blood pressure and lasix for the water retention (which did nothing to help establish my milk supply, sadly) and we were told to have Tory's bilirubin levels checked at Children's hospital every other day. We took Tory to have her bilirubin levels checked on Wednesday and Thursday and on Friday morning, a nurse came to our home to set up a special bili light unit which Tory was to stay under for the next day and a half or so. We had to leave her under the lights except to feed her and she was also wrapped in a little "glow worn" vest around her middle. Breastfeeding was not going well, both DH and I were overwhelmed and exhausted, we were supplementing with bottles of formula and the heat was oppressive. I was feeling increasingly worse, but put it down to the heat and exhaustion.
On Sunday, Tory was finished with the bili lights and we gave her a bath. We'd been in the house all week and we decided to go shopping. We pulled ourselves together, packed Tory up and headed to the local mall. We'd been walking around in a drugstore for a little while when I started feeling very strange. It's hard to explain, but I just didn't feel right. We went home and DH checked my blood pressure. It had spiked really high. We waited a bit to see if it came back down with some rest, but it didn't. DH called the hospital and we were told to come in.
At the hospital, my blood pressure was still very high and they did some labs and determined I had developed preeclampsia. I was admitted and started on mag sulfate. I hated the mag. It made me feel like I was going to come right out of my skin. I felt completely out of it and so foggy I couldn't even carry on a conversation, but my body was so restless and uncomfortable, I thought I didn't know what to do with myself. I started to panic that Tory would be hungry by now but I just couldn't nurse her. I couldn't even hold her. I watched as DH gave her a bottle and felt awful. She was getting too many bottles and too much formula and I felt so defeated. I couldn't stand the restlessness anymore and finally complained. I was given something to help with the restlessness, perhaps a sedative, I don't remember anymore, and it helped. I think I slept. It was Sunday evening, one week to the day since Tory was born, and here I was back in the hospital. I spent the first few days in and out of it, I think because I was just so exhausted. Tory stayed with me and DH was also able to stay and care for her. I felt resentful that I had developed preeclampsia in spite of the fact that Tory's birth had been induced to avoid this very thing. I wondered if we could have just let her birth come spontaneously, since the induction hadn't prevented preeclampsia anyway. Later, someone remarked "Wow, it's a good thing you were induced before the preeclampsia developed!" I hadn't thought of it that way. But they were right. At least, my preeclampsia didn't involve my baby.
I was in hospital for a week and sent home with new medications. In the weeks and months that followed, DH returned to work and I continued to struggle to breastfeed Tory and get sleep where I could. I was still exhausted and I was very disappointed how Tory's birth and first weeks had unfolded. I started to lose interest in everything and had decided I was an awful mother. I told DH I wanted him to stay home and care for Tory and I would go to work. When I saw pregnant women, I honestly pitied them. I swore we would never have another child and was so convinced of this that I felt guilty and sorry for Tory that she would be raised an only child. I became so miserable that I felt like I was moving through a thick fog and only looked forward to when Tory was someday start college and all this struggle to breastfeed, the sleepless nights, and the guilt and disappointment over her birth would be far behind me. When Tory was about 3 months old, I was diagnosed with severe PPD and started medication and therapy. It made all the difference and I started to feel like a human being again. Even happy. Things improved steadily after that.
My experience with preeclampsia has put a cloud of fear over each of my subsequent pregnancies. I've tried baby aspirin therapy, vitamin C and E therapy, the Brewer diet and I can't remember what else. I've had problems with my blood pressure with each of my pregnancies, but thankfully have not had a repeat of preeclampsia. And, of course, I worry for when my daughters become pregnant some day. I hope, by that time, we will understand preeclampsia better and be able to prevent it completely.
Subscribe to:
Posts (Atom)


.jpg)



